The EMI plan was designed for CCSD employees and eligible retirees that reside in the rural areas of Clark County, including Mesquite and Logandale, as well as neighboring regions in Utah and Arizona. Although the EMI plan is no longer open to new members, its existing participants are grandfathered into this plan. EMI plan members can elect to move into our other plans during an open enrollment period.
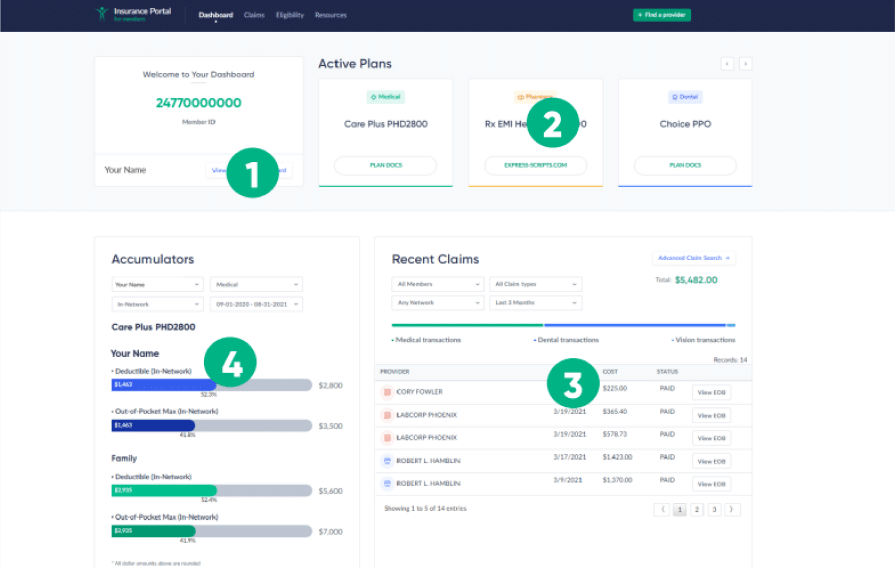
Visit EMIHealth.com or download the EMI Health to manage all your benefits in one place.