Open Enrollment closed Aug 25. Any new plan changes take effect Oct 1. Contact THT with any concerns.
What is open enrollment?
Open enrollment is your once-a-year opportunity to make any changes to your health plan selections. This includes changing your medical, supplement, dental, or vision plan, as well as adding or removing any dependents.
When is open enrollment?
Open enrollment begins August 1st at 12am and runs through August 25th at 11:59pm.
When do my open enrollment selections go into effect?
The elections you make during annual Open Enrollment become effective October 1, as long as all enrollment requirements are completed on time. If you are a summer new hire, your new hire enrollment period may overlap with the annual open enrollment period. Refer to the New Hire Enrollment page for more information.
Is participation in open enrollment required? / What if I don’t participate in open enrollment?
No, participation is not required. If you do not participate in open enrollment, your same plan selections and dependents will carry over into the new plan year. You will not be able to make any plan changes until the next open enrollment period or you experience a Qualifying Life Event.
Choosing Your Plans
We understand that health benefits can quickly become confusing. To help you make informed decisions, we’ve created these videos that walk through each of our plans and highlight the key differences. For more information, visit the Medical, Supplement, Dental, and Vision pages.
The 2024-25 Benefits Guide also includes all relevant information.
Medical Plans
Supplement Plans
Dental Plans
Vision Plans
2024-2025 Benefit Changes
THT evaluated its benefit offerings and made adjustments to provide additional value, simplify specific coverages, and remain in compliance with new regulations. Refer to the table below for all changes.
Advantage Plan Changes
| Benefit | New | Old |
|---|---|---|
| Tier 1 (In-Area) Deductible (individual / family) | $1,650 / $3,300 | $1,500 / $3,000 |
| Tier 2 (Out-of-Area) Deductible (individual / family) | $3,300 / $6,600 | $3,000 / $6,000 |
| Tier 1 (In-Area) Out of Pocket Maximum (individual / family) | $7,500 / $15,000 | $7,000 / $14,000 |
| Tier 2 (Out-of-Area) Out of Pocket Maximum (individual / family) | $9,200 / $18,400 | $7,000 / $14,000 |
| Tier 2 (Out-of-Area) Urgent Cares & Walk-in Clinics now covered at Tier 1 benefits | Member pays 20% after Tier 1 deductible | Member pays 50% after Tier 2 deductible |
| Out-of-network Urgent Cares & Walk-in Clinics now covered at Tier 2 benefits | Member pays 50% after Tier 2 deductible | Member pays 100% |
| Telehealth / MDLive | Member pays 20% after deductible | Member pays 0%, deductible waived |
Signature Plan Changes
| Benefit | New | Old |
|---|---|---|
| Tier 2 (Out-of-Area) Out of Pocket Maximum (individual / family) | $9,200 / $18,400 | $7,500 / $15,000 |
| Tier 2 (Out-of-Area) Urgent Cares & Walk-in Clinics now covered at Tier 1 benefits | $30 copay | Member pays 50% after Tier 2 deductible |
| Out-of-network Urgent Cares & Walk-in Clinics now covered at Tier 2 benefits | Member pays 50% after Tier 2 deductible | Member pays 100% |
| Deductibles for newborns | For first 5 days following birth, deductible does not apply for facility and physician charges. | For first 5 days following birth, deductible does not apply for facility charges. |
| Mammograms | The first mammogram of the plan year is covered at 100% regardless of diagnosis billed. | Only mammograms billed as routine/preventive are covered at 100%. |
| Colonoscopies | The first colonoscopy of the plan year is covered at 100% regardless of diagnosis billed. | Only colonoscopies billed as routine/preventive are covered at 100%. |
| Bereavement Counselling | $10 Copay | 20% after deductible |
Dental PPO Changes
| Benefit | New | Old |
|---|---|---|
| Out-of-network coverage for Class 1: Diagnostic / Preventive Services | 80% | 100% |
| Out-of-network coverage for Class 2: Basic Services | 50% | 80% |
| Out-of-network coverage for Class 3: Major Services | 50% | 60% |
| Out-of-network coverage for Class 5: Implants | 50% | 60% |
$0 Copay - Providers
-
$0 Copay for Covered Services:
You will no longer have to worry about any out-of-pocket expenses for covered services during your visits. Your copay for all covered services will be $0, making it easier for you to focus on your health without financial stress. Advantage plan members must meet their deductible before they receive the $0 copay benefit.
Note: Many providers offer “Concierge” packages or services. These are not covered by THT.
-
Quick Appointment Scheduling:
We understand the importance of timely access to care. These providers are committed to helping you get quick appointments for the care you need.
-
Which providers are included?
Available services currently include primary care, pediatrics, and behavioral health office visits. These providers are committed to expediting appointments for THT members. Physical Therapy providers are launching 10/1/24. View the growing provider list at ththealth.org/health-investment.
$0 Copay - Mobile Urgent Care
In-Home Urgent Care Visit
DispatchHealth, DoctorRoo, or IncrediCare
Effective 5/18/2024: $0 Copay for Signature Plan members. Advantage plan pays $0 after meeting the deductible.
Use when you’d like Urgent Care to come to you. The house call team arrives at your door.
- DispatchHealth – (702) 329-2093 (THT-dedicated line)
- DoctorRoo – (888) 888-9930
- IncrediCare – (725) 867-8144



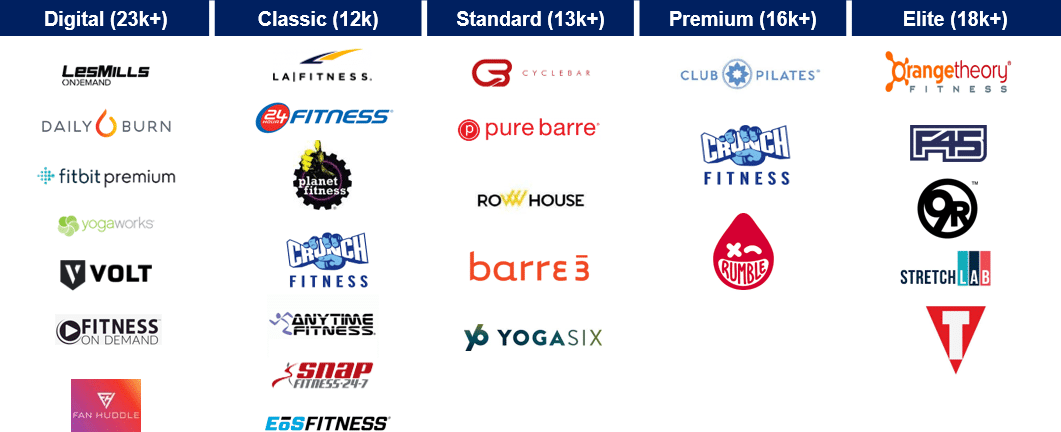
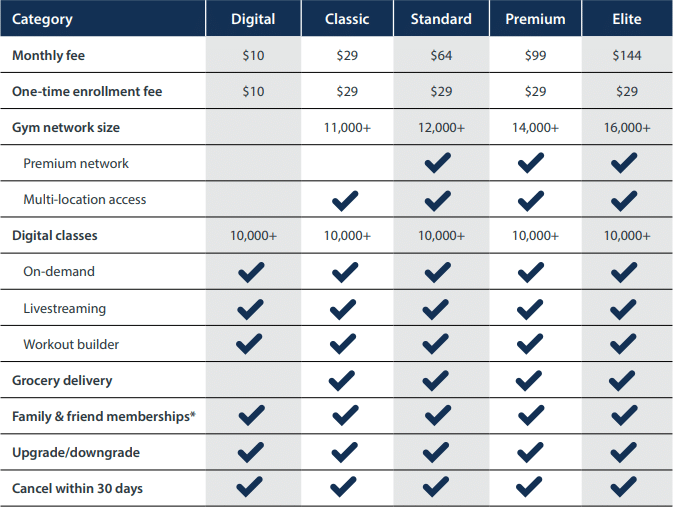
One Pass Select™ Fitness Membership
Flexible, accessible health options
One Pass Select is a subscription-based program that provides access to gyms, boutique fitness studios, thousands of online workouts, and your perks services with one monthly membership. Starting 10/1/24, you can sign up for a plan and start accessing gyms across the country. One Pass Select will bill you directly for your monthly membership fee, which depends on the membership tier that you select. The higher tier you select, the more facilities and perks you can access.
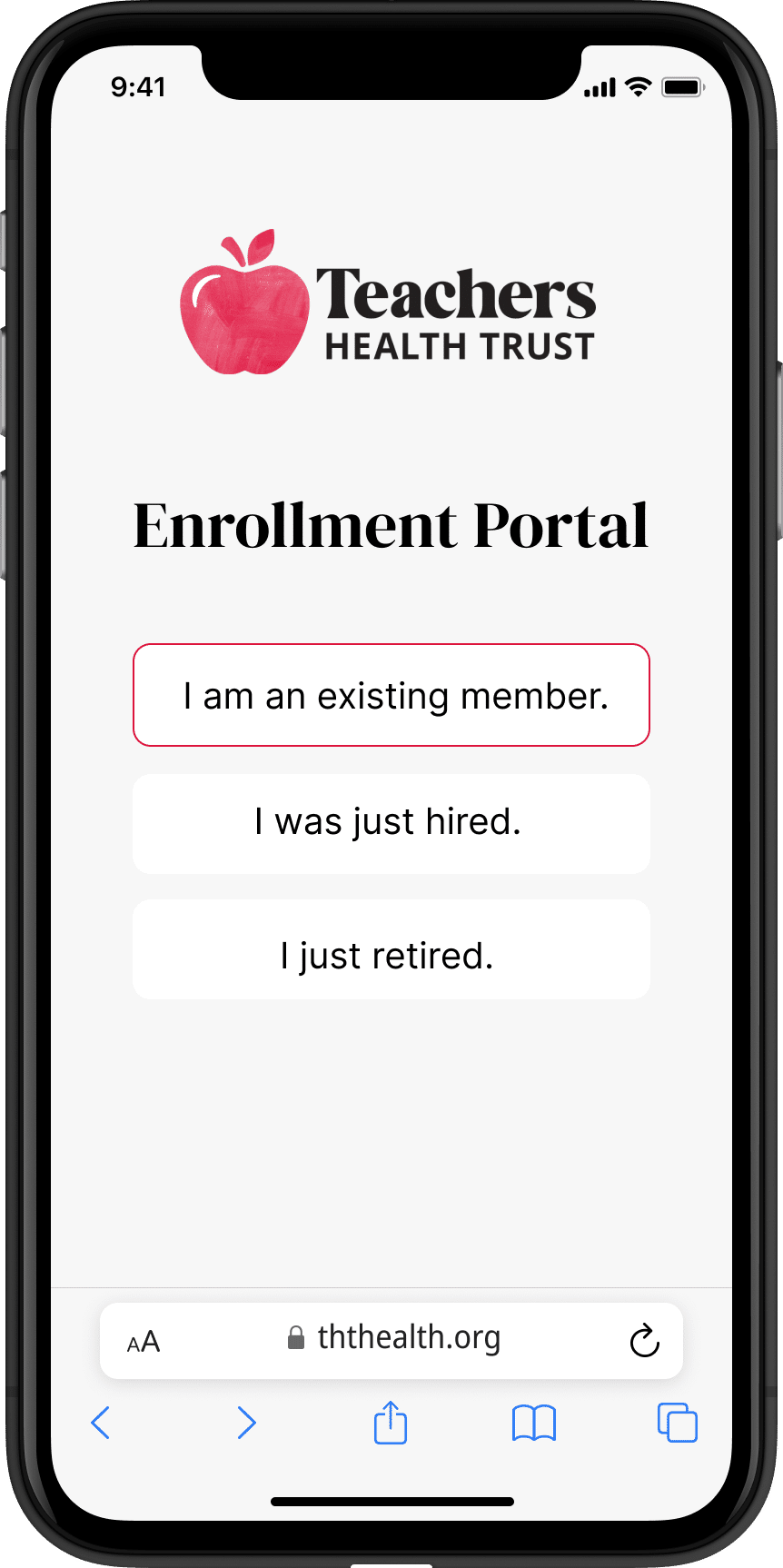
Enrolling is Easy on Desktop and Mobile!
- Enroll online on at enrollment.ththealth.org
- Select the appropriate member type
- Verify your identity and update your info
- Select your plans and add / remove dependents
- Double check your selections and submit
Upon submitting your selections, you will immediately receive an enrollment summary to the email address on file. Once processed, you will receive a separate confirmation email. Please retain these files for your records and contact us immediately if you have any concerns.
For COBRA participants:
COBRA participants wanting to make changes will make their selections via a mailed enrollment form from WEX Inc. Alternatively, you may print this form and postmark it by August 25.