Enroll or opt out within 31 days of your hire date. Otherwise, you will be automatically enrolled.
Overview
What is Teachers Health Trust (THT)?
Teachers Health Trust is the health plan for all educators and licensed professionals of Clark County School District. Unlike other employers, whose health benefits are through the HR department, we are your source for any questions/concerns related to your health benefits.
How do I manage my health benefits?
As a THT member, you will use the THT member portal for everything regarding your health benefits. It is possible to make elections/requests in HCM, however, those elections/requests are not valid.
What else makes THT different?
Teachers Health Trust is a self-funded plan, meaning more of your dollars go towards benefits.
When do my benefits start?
- Summer New Hires (Hired in July/August): Your health benefits will begin on September 1. (Deductibles reset October 1st).
- All Other New Hires: Your health benefits will begin on the 1st of the following month.
Coming Back from a Leave of Absence (LOA) or for Critical Labor Shortage (CLS)?
Participants who are coming back from a Leave of Absence or for Critical Labor Shortage will need to reenroll in their benefits through the Teachers Health Trust Enrollment Portal the same way a new hire would. Benefits will be effective the first of the month following your “re-hire” date. Those who were on a Family Medical Leave (FMLA) will have no break in coverage and will not need to reenroll.
Choosing Your Plans
We understand that health benefits can quickly become confusing. To help you make informed decisions, we’ve created the below videos that walk through each of our plans and highlight the key differences. Alternatively, review all plan information on the respective coverage pages.
- Medical / Pharmacy – Signature, Advantage (High-Deductible Plan), Spousal / Domestic Partner Supplement Plan, or Hospital Supplement Plan
- Dental – Cigna PPO or Cigna HMO
- Vision – VSP Standard Vision or VSP Vision Plus
- Life – $50,000 Term Life Benefit
- Employee Assistance Program – Additional Behavioral Health Services
- Wellness & Weight Loss Programs
The 2024-25 Benefits Guide also includes all relevant information.
Medical Plans
Supplement Plans
Dental Plans
Vision Plans
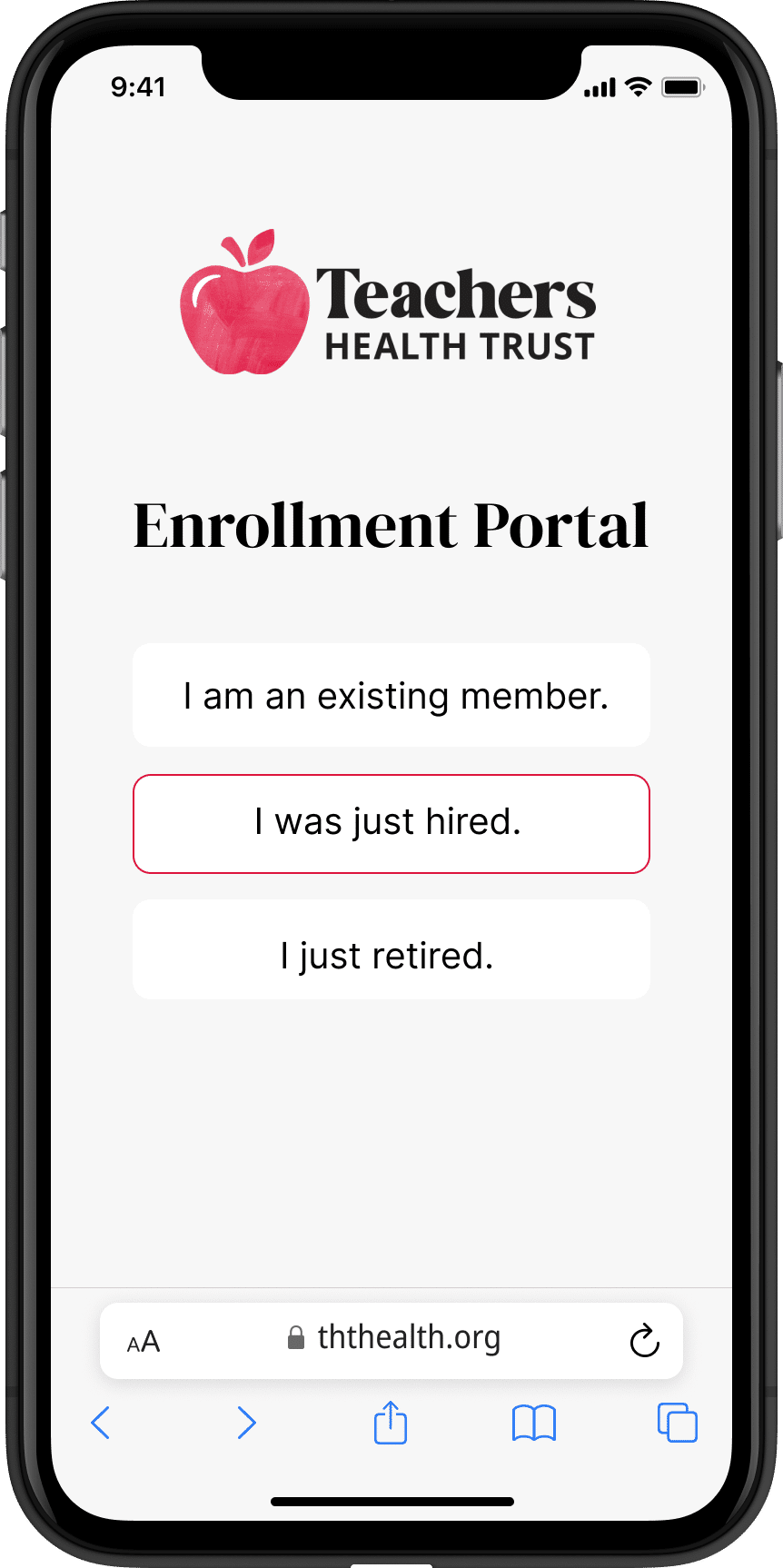
Enrolling for Benefits as a New Hire / Rehire
Enroll or “Opt Out” within 31 Days of Starting Work
You can enroll or opt out beginning on your first day using the THT enrollment portal. If also enrolling dependents, supporting must also be uploaded within 31 days of your start date. See required documents for dependents.
After 31 days, you will be enrolled by default.
Members who do not enroll or opt out within 31 days of their hire date will be automatically defaulted in the Signature Plan with Dental HMO and VSP Standard. The appropriate premiums will be deducted from your paycheck. Visit the premiums page to view the current rates. After the new hire enrollment period, members will be unable to make changes until the next Open Enrollment Period or if they experience a qualifying life event.
Enrolling is Easy on Desktop and Mobile!
- Enroll online on at enrollment.ththealth.org
- Select the appropriate member type
- Verify your identity and update your info
- Select your plans and add / remove dependents
- Double check your selections and submit
Upon submitting your selections, you will immediately receive an enrollment summary to the email address on file. Once processed, you will receive a separate confirmation email. Please retain these files for your records and contact us immediately if you have any concerns.
Making Future Changes
- After your initial new hire enrollment, you can make any changes during our Annual Open Enrollment (typically in August) to take effect the following October 1.
- Members who experience a Qualified Life Event (QLE) can submit a request within 30 days of the event to add or remove dependents or change enrollment status, as applicable.
- Our plan year begins October 1 and ends September 30. (Your benefit selections will carry over automatically unless you change them; however, your premium may change.)